CPT Code 00812: Anesthesia Billing for Screening Colonoscopy
September 5, 2025
Anesthesia billers ensure healthcare providers receive precise compensation for their care during medical procedures. Accurate coding is critical in anesthesia billing because it enables complete reimbursement, maintains compliance with healthcare regulations, and prevents claim denials.
CPT code 00812 covers anesthesia services provided during lower intestinal endoscopic procedures, particularly screening colonoscopies. This code helps providers document anesthesia services accurately and secure reimbursement as part of the overall procedure, supporting compliance and effective financial management within healthcare practices.
Correct anesthesia coding streamlines the billing process, reduces errors, and promotes transparency among providers, payers, and patients. Without accurate coding, hospitals and clinics risk financial losses and operational challenges.
This blog clarifies the specifics of CPT Code 00812, which providers use for anesthesia billing during screening colonoscopies. By understanding this code’s purpose and proper application, healthcare professionals can improve billing accuracy and optimize revenue cycles for these essential procedures.
CPT Code 00812 clearly reports the anesthesia services performed during a screening colonoscopy. It was created to reflect the distinct nature of screening procedures, which are preventive rather than diagnostic or therapeutic.
According to the American Medical Association (AMA), CPT 00812 is known as:
“Anesthesia for lower intestinal endoscopic procedures, endoscope introduced distal to the duodenum; screening colonoscopy.”
Providers use CPT code 00812 specifically when they administer anesthesia during a screening colonoscopy performed as a preventive measure, with no signs or symptoms present. Depending on current guidelines, they often recommend this procedure for patients over 45 or 50.
Anesthesia Doctors bill for their services using CPT 00812 when a patient comes for a routine colon cancer screening with no prior gastrointestinal symptoms or diagnosis. It is essential to differentiate this from codes used for colonoscopies that are diagnostic or therapeutic in nature.
Differentiation from Other Anesthesia CPT Codes
The accurate anesthesia CPT code ensures correct billing and reimbursement and avoids claim denials or audits. CPT 00812 especially applies to anesthesia provided during a screening colonoscopy for patients without high-risk factors. However, providers need to understand the distinctions due to its similarity to other codes.
Commonly Confused Codes:
Billing Scenario:
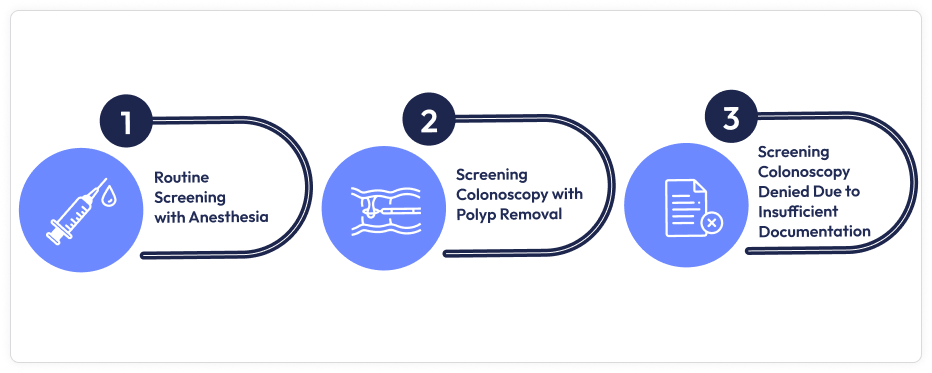
A 55-year-old patient with no personal or family history of colorectal cancer undergoes a routine screening colonoscopy. The provider administers anesthesia solely for this preventive screening, no polyps are found or removed.
In this case, the accurate anesthesia code is CPT 00812, as the procedure is a routine screening without high-risk indicators or therapeutic intervention. Choosing CPT 00810 or CPT 00813 would be inappropriate and could lead to claim denial or overbilling.
Conversely, the colonoscopy becomes therapeutic if the provider discovers and removes a polyp during the procedure. In that case, the appropriate anesthesia code changes to CPT 00810.
Providers must base code selection not just on the procedure type, but also on why the procedure was performed and what occurred during it. Clear documentation of the patient’s history and the procedural intent screening vs. diagnostic/therapeutic is essential for choosing the correct CPT code and ensuring smooth billing.
Understanding how CPT 00812 fits alongside related anesthesia codes is crucial for correct billing and avoiding rejections.
CPT 00812: CPT codes describe anesthesia for a screening colonoscopy performed on an asymptomatic patient without prior gastrointestinal GI symptoms or therapeutic interventions. It is used when anesthesia is medically necessary for a preventive colonoscopy.
CPT 00811: CPT code covers anesthesia for diagnostic and therapeutic colonoscopy procedures. Assign code 00811 when the colonoscopy is performed due to symptoms (e.g., bleeding, pain) or involves therapeutic interventions like biopsy or polyp removal, even if it began as a screening.
CPT 00810: Anesthesia for upper gastrointestinal endoscopic procedure (e.g., esophagoscopy)
CPT 00813: anesthesia for protologic procedures, which are different from colonoscopies.
Key Point: If a screening colonoscopy becomes a therapeutic procedure during the same session, bill CPT 00811, not 00812.
Establishing medical necessity and thorough documentation are critical for proper reimbursement and compliance when billing anesthesia for a screening colonoscopy under CPT Code 00812.
Anesthesia practitioners must document detailed information that supports the need for anesthesia during the procedure. It includes:
Complete documentation ensures payers understand that anesthesia was medically needed and not routine.
While billing for anesthesia services during a colonoscopy, especially under CPT Code 00812 (anesthesia for routine screening colonoscopy), it is crucial to understand how the type of anesthesia administered influences coding and reimbursement. The two most common methods are:
MAC is the most frequently used anesthesia method for colonoscopy. It involves moderate to deep sedation, often with agents like propofol, allowing patients to remain responsive while maintaining comfort and safety.
Billing Consideration:
Although CPT 00812 does not change based on whether MAC or general anesthesia is used, payers may require justification when MAC is chosen, especially for low-risk patients undergoing routine screenings. To support the medical necessity of MAC, providers should document:
Failing to include these details can lead to claim rejections or audits, as MAC may be seen as excessive without clinical justification.
While less common, general anesthesia may be warranted in specific situations, such as:
If general anesthesia is used, detailed documentation is even more critical. Since general anesthesia involves greater risk, higher intensity care, and airway management, payers often scrutinize these claims closely. Providers should document:
CPT 00812 only describes the procedural context (routine screening colonoscopy) and does not distinguish between anesthesia types. However, reimbursement and claim acceptance often hinge on medical necessity, mainly when a higher level of sedation is used for a low-risk procedure.
Billing the anesthesia services can be complex, like others. As a healthcare provider, you must know how to keep things on track. You can follow these anesthesia billing guidelines to ensure a smooth anesthesia billing process and increase your practice’s reimbursement rates.
Use CPT Code 00812 when:
Do Not Use CPT 00812 if:
ICD-10 Diagnosis Codes
Accurate ICD-10 codes are crucial to justify the medical necessity of the anesthesia service:
For screening colonoscopy, use ICD-10 codes that reflect asymptomatic screening, such as:
Do not use codes showing symptoms or disease (e.g., K52.9 for unspecific colitis) with CPT 00812, as this would suggest a diagnostic or therapeutic procedure requiring CPT 00811.
Modifier explains the provider’s role and scenarios:
Preventive Service Modifier
Modifier 33 applies to the colonoscopy procedure code (not the anesthesia CPT 00812) to indicate a preventive service for insurance purposes, often resulting in waived patient cost-sharing.
Billing anesthesia for screening colonoscopies using CPT 00812 can differ depending on the patient’s clinical situation and payer policies. Here are some typical scenarios to keep in mind:
Medicare and commercial insurers have different but equally essential guidelines for covering anesthesia services during screening colonoscopies. Understanding these policies helps providers ensure accurate billing, proper documentation, and timely reimbursement while minimizing patient costs and avoiding claim denials.
Coverage: Medicare covers anesthesia services for screening colonoscopies when medically necessary. Due to preventive service rules, these anesthesia services typically involve no patient cost-sharing, provided the colonoscopy is a proper screening procedure.
Billing: Use CPT 00812 to bill anesthesia for screening colonoscopy.
Important: Modifier 33 (preventive service) applies only to the colonoscopy procedure code, not the anesthesia code. Ensure all modifiers are applied correctly to reflect the nature of the service.
Documentation:
Medicare requires comprehensive anesthesia documentation, including:
Denials: Claims may be denied if the colonoscopy is diagnostic or therapeutic (e.g., polyp removal) but billed as screening. Lack of clear documentation supporting the screening intent or medical necessity of anesthesia can also lead to claim denials.
Variability: Commercial insurers may have distinct requirements and reimbursement policies. Some may bundle anesthesia into the colonoscopy, while others pay separately.
Preauthorization: Many commercial plans require preauthorization for anesthesia during colonoscopy screening.
Modifiers: Use accurate anesthesia and preventive service modifiers according to the insurer’s guidelines.
Patient Responsibility: Some commercial plans apply copays or deductibles even if Medicare waives them.
Here are some tips for the providers on what they should do in both of the cases mentioned above:
Accurate documentation and clean claims are the backbone of successful healthcare billing.
Here are some tips that will help:

Include the right anesthesia provider modifier, such as:
For the colonoscopy code, not 00812, add Modifier 33 to indicate it’s a preventive service and help waive patient cost-sharing where applicable.
Provide ongoing training on:
Correct and compliant billing of CPT Code 00812 for anesthesia services during screening colonoscopies requires a clear understanding of the procedure’s intent, proper documentation, accurate code selection, and correct modifier usage. Distinguishing screening from diagnostic or therapeutic procedures is crucial, as is aligning documentation across all providers and using the appropriate ICD-10 codes and anesthesia modifiers to support claims.
To ensure complete reimbursement and avoid denials, providers and billing staff must consistently verify medical necessity, record precise anesthesia times, and stay proactive with payer-specific guidelines. Moreover, keeping up to date with evolving coding rules is not just best practice—it is essential for maintaining billing accuracy and protecting revenue integrity in anesthesia services.
Need help optimizing your anesthesia claims for screening colonoscopy?
Contact Utha Billing Services for expert coding, documentation, and billing support to maximize your reimbursement and reduce claim denials.
Book an appointment today at Utha Billing Services for a free consultation!